The COVID-19 Vaccines
/Research teams around the world are working to develop a vaccine against the virus causing the current COVID-19 pandemic. Given the severity of the disease, vaccines are urgently needed to control this virus. Immunization can help to slow the spread of the virus, reduce morbidity (rate of having the disease), mortality (death rate), and may also help prevent development of severe symptoms for those infected.
Once the sequence of the COVID-19 virus was published in January 2020, scientist have rushed to use the information to design a vaccine. To date, out of the nearly 100 vaccines being developed, eight are already in clinical trials (see WHO landscape of COVID-19 candidate vaccines).
This blog post will explain how these different vaccines are designed to work.
Before I dive right into, let’s start with the simple question – what is a vaccine?
What is a vaccine?
A vaccine is a harmless variant or derivative of a pathogen (which can be a virus, bacteria or other organism that causes disease). The aim of the vaccine is to trigger the immune system to produce antibodies, a type of protein that recognise the vaccine components as foreign and targets it for destruction. The immune system then acquires a ‘memory’ for that particular pathogen, so when a vaccinated individual does become infected, their immune system is able to trigger a rapid and strong response to protect them from that pathogen. In contrast, medical drugs work by fighting the infection once you have it.
The first use of vaccination was against smallpox, a devastating disease that caused death, blindness and disfigurement worldwide for centuries, before global vaccination resulted in its eradication in the late 1970s. Since then, vaccination has been successful in developing immunity against many infectious diseases that would otherwise kill or incapacitate large numbers of people worldwide. Vaccines are particularly important for protection against disease causing viruses where there are no drugs available to cure the disease. Note that unlike bacterial infections, antibiotics cannot be used to treat viral infections. However, antibiotics are used to treat the secondary infections that usually follow, such as bacterial pneumonia in the case of HIV.
Knowing the structure of the virus, its genome and how it gets inside a cell to reproduce, are essential in the design of antigens that make up the vaccines. Antigens are the variant or derivative of the virus that can be used to elicit the immune response.
The COVID-19 virus
COVID-19 (short for Coronavirus Disease 2019) is caused by the SARS-CoV-2 coronavirus. It has a single-stranded RNA genome (the genetic information) surrounded by a protective protein coat called a capsid, and a membranous envelope, as illustrated in Figure 1.
On the outer membranous envelope are spike proteins that stick out of the surface of the virus giving the appearance of a crown, hence their name (corona is Latin for crown).
As mentioned in previous posts, viruses are intracellular obligate parasites. This basically means that they need to get into a cell in order to take it over to make more viruses. (See previous post on ‘what are viruses’ and ‘reproduction of viruses’ for full details). Some viruses, like the SARS-CoV-2 virus, require a protein, such as a receptor, found on the surface of the susceptible host cell to help them get inside it.
SARS-CoV-2 enters the cell by attaching its spike proteins to the angiotensin-converting enzyme 2 (ACE2) receptor, as illustrated in Figure 2 below. The ACE2 receptor is found on the surface of the cells in several organs, including the heart, kidney and lungs (the primary target of SARS-CoV-2), and regulates the function of these cells. Once attached to the ACE2 receptor, the SARS-CoV-2 virus enters the host cell and takes advantage of the molecules inside to make more viruses.
Designing the COVID-19 Vaccines
In order for a vaccine to be effective, it must be able to generate a rapid and strong immune response when the vaccinated person is exposed to the target pathogen. Vaccines are currently being developed using various types of antigens to generate protective immunity against the SARS-CoV-2 virus. The four main types of vaccines are described below.
Vaccine Type 1: The whole virus
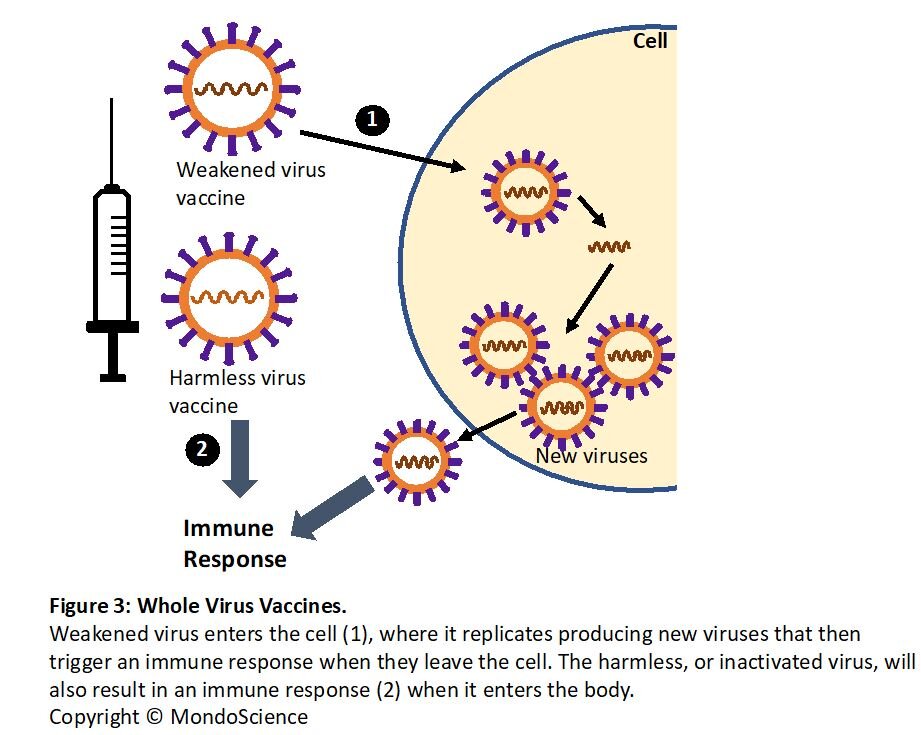
This type of vaccine uses the SARS-CoV-2 virus itself that has either been made harmless, using chemicals or heat, or has been genetically altered to weaken it so the virus is unable to cause the disease.
As shown in Figure 3, once inside the body, the weakened (also known as attenuated) virus enters the cell, but replication is less efficient due to the genetic modification. This also makes it less virulent (less likely to cause disease) yet still able to trigger an immune response. On the other hand, the harmless (inactivated) virus is able to instigate an immune response without the possibility of causing COVID-19.
Many vaccines are made using harmless or weakened virus such as those against measles, mumps and rubella, but extensive testing is required to ensure that they are safe. Use of live SARS-CoV-2 virus for a vaccine is unlikely due to the risk of developing COVID-19. Phase I/II clinical trials using inactivated virus is currently underway in China.
Vaccine Type 2: Nucleic acid
These vaccines consist of DNA or RNA, the two forms of nucleic acids that encode the genetic information needed to make an organism. The DNA or RNA in these vaccines must enter the cell (see Figure 4) to produce the viral proteins that will then act as antigens to trigger the immune response.
In most cases, the nucleic acids (DNA or RNA) used for these vaccines encode the spike protein, or part of it, as this protein is essential for the SARS-CoV-2 virus to enter the cell. Antibodies that can target the spike protein could potentially block the ability of the virus to enter the cell, stopping it from replicating, thereby preventing it from causing COVID-19.
There are currently no licensed nucleic acid vaccines, however, this technology is developing fast. Three groups, including Moderna, have recently started testing their RNA and DNA vaccines in clinical trials. In addition, Imperial College London, UK, have had promising results in animal studies using an RNA vaccine, and will move forward with human trials soon.
Vaccine Type 3: Protein based
Proteins purified from the SARS-CoV-2 virus, or generated in the lab, are used in this type of vaccine (see Figure 5). Again, most groups are concentrating on the viral spike protein or its key subunits. Other groups are working on producing viral-like particles, which look like the virus but without the genetic material that make it harmful (almost like an empty shell).
Protein based vaccines have been generated against another coronavirus, the SARS-CoV-1 virus, that causes Severe Acute Respiratory Syndrome (SARS). However, testing in monkeys has shown the vaccine to protect against infection in some cases, and unfortunately enhancing the viral infection in others. This type of vaccine may also require immune-stimulating molecules to be effective in triggering a strong immune response.
Vaccine Type 4: Viral vector
Viral vector vaccines are based on genetically engineered viruses that are used as a carrier (or vector) for part of the SARS-CoV-2 genetic code. These viral vectors have been weakened and will either retain their ability to replicate in the cell or not. The viral vector, with the addition of the SARS-CoV-2 genetic code, easily infects the cell where expression of the SARS-CoV-2 proteins can occur. These vaccines have the advantage of inducing a rapid and strong immune response.
Groups have taken part of the SARS-CoV-2 genome that codes for the spike protein and cloned it into weakened viruses, such as the measle virus. Once inside the body the virus is able to replicate and produce the viral spike proteins in the cell (see Figure 6). A similar approach was used for the recently approved Ebola vaccine.
Other groups are developing their vaccines in non-replicating viral vectors, that can enter the cell to produce the viral spike proteins but cannot make more copies of itself. Clinical trials in the UK have started using such a vaccine developed at the University of Oxford. Their vaccine consists of the genetic information of the SARS-CoV-2 spike protein inserted into a weakened non-replicating adenovirus (a virus which causes the common cold).
Summary
Vaccines play a critical role in protection against infectious diseases. However, there are currently no vaccines that can protect against emerging diseases such as HIV/AIDS and SARS.
There are vaccines available against some viruses, such as measles, and this helps reduce the incidence of the disease and chances of an outbreak. Today, numerous research groups around the world are using different approaches and new technologies to develop candidate vaccines against COVID-19.
Most vaccine design concentrates on using the SARS-CoV-2 spike protein as an antigen in the hope to trigger the immune system to produce antibodies against the it. The immune system of the vaccinated person will develop a ‘memory’, so that if they are later infected with the actual SARS-CoV-2 virus, their immune system is able stop the virus from entering the cells and thereby prevent them from developing COVID-19.
Early phase trials have now started for a handful of COVID-19 vaccines with the hope of finding one that is both highly effective and safe. The vaccines are likely to come too late to prevent a second wave of the COVID-19 pandemic, however, they would prove useful in the future to help in the elimination of this virus. In addition, technologies and lessons learned now will help us to respond rapidly to any future sudden outbreak by an emerging virus.
If you enjoyed reading this, please like, share or leave a comment.